Nannette Ruelle is watching three numbers tick downward as the year comes to a close. The first is the number of doses left in her Advair inhaler, which she normally uses three times a day to control her asthma. As of Nov. 17, she had 35 remaining. The second is the number of pills in her bottle of Gabapentin, which her doctor told her to take three times daily for chronic neuropathic pain in her feet and ankles. She had three as of Nov. 17.
The third is the number of days left until she can refill those prescriptions: 44. She was kicked off her Arkansas Works health insurance in September and will be locked out until Jan. 1.
Ruelle, 38, lost her coverage at the end of August due to Arkansas's new requirement that certain Medicaid beneficiaries report their work hours to the state. For the past two-and-a-half months, she's been carefully rationing both her medications, allowing herself a Gabapentin only when the nerve pain becomes so bad she fears she won't be able to do her job. Ruelle works 25-35 hours a week at a chain restaurant in Little Rock, where she makes $9 an hour.
"It's some serious stuff. They're just playing around with people's lives, and I don't think it's fair," she said in a recent interview. "What if I wake up one morning and I can't even function because my feet are hurting and I have nothing left?"
Ruelle said she first recalled hearing about the requirement in May, when she was working a minimum wage job at a different restaurant. The instructions on the notice she received from the state Department of Human Services were confusing, but she tried to do what the letter demanded.
"What happened was that I got my information and I tried to fax it to them. The fax wouldn't go through, so I tried calling them, and I never got an answer on the phone. I went up there and they were out of the office," she said.
When she got no reply after leaving voicemails and visiting her local DHS office, Ruelle said, she gave up. "I just quit trying, because you can only try so many times before it's like, 'OK, you're closing the door in my face.' "
Over the last three months, DHS has removed 12,277 people from Arkansas Works — the state's Medicaid-funded insurance program for low-income adults — for not reporting their work hours. Thousands more will likely join them in December. The rule, which began for the first subset of beneficiaries in June, requires able-bodied adults under age 50 to report at least 80 hours of "work activities" each month. (In 2018, the requirement applied only to those ages 30-49, but it will begin including 19- to 29-year-olds in 2019.) Those who don't comply for any three months in a calendar year are kicked off Arkansas Works and locked out until the new year begins.
Ruelle's attempts to reach DHS were unsuccessful in part because the agency only allows people to report their work hours through a website, rather than by fax, phone or mail. This online-only requirement is unlike any other reporting required by DHS. The agency places no such restriction on the way beneficiaries submit other information, such as a change of address — just their work hours.
DHS first sends Arkansas Works recipients who must meet the work requirement a letter directing them to https://access.arkansas.gov. As of Nov. 16, that URL sent users to a general DHS landing page containing information about voter registration, not health insurance. From the landing page, a beneficiary must navigate a series of menus to reach a login page, where he or she is prompted to create a new account. (Doing so requires an active email address.) Then, the user must locate a unique "reference number" contained on the letter from DHS "to link your online account to your healthcare coverage." Only then can the beneficiary enter work hours.
Ruelle said she tried to follow this process but ran into problems there, too. "You set up passwords and stuff, and the passwords won't work. ... It would tell you your user ID was invalid and then it would tell you your password's invalid."
"I tried to call them to help me go through all that stuff, and I couldn't ever get a response," she said.
DHS spokeswoman Marci Manley said local offices have resources on hand to help beneficiaries report their hours. "We have computers and kiosks available, and a staff person can offer one-on-one assistance," she said.
The Arkansas experiment
Arkansas is the first state to implement a work requirement in its Medicaid program. Kentucky attempted to launch a similar rule earlier this year, but a federal judge in the District of Columbia sided with a group of plaintiffs and blocked the policy in June before it went into effect. A lawsuit challenging Arkansas's work requirement is now before the same judge, but a ruling isn't expected until 2019.
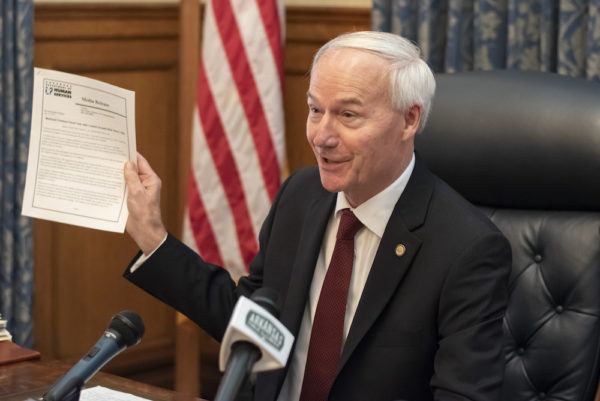
Governor Hutchinson, who received permission from the Trump administration in March to implement the work requirement, has said the "common-sense" policy is saving taxpayers money and incentivizing Arkansas Works beneficiaries to move up the economic ladder. He's pointed to an unemployment rate near record lows as evidence jobs are available for anyone willing to work. Beneficiaries also get some credit for other activities, like school, volunteering or searching for jobs. The state Department of Workforce Services operates dozens of centers statewide that stand ready to help people find employment or training, Hutchinson says.
The governor has also noted the broad exemptions built into the program. Anyone with a dependent child in the house is exempt from reporting, as are full-time students and certain people with high-end medical needs, among other categories. DHS also automatically exempts people whose incomes were at least $680 per month when they first applied for Arkansas Works, under the assumption they're working enough already. The requirement applies only to the "Medicaid expansion" population under Obamacare, thus excluding anyone receiving federal disability payments (Supplemental Security Income, or SSI) and those in other "traditional" Medicaid categories.
In September, when the work requirement first began cutting people from the Medicaid rolls, Hutchinson listed reasons why people might not be reporting. "One, they could have ... obtained other insurance coverage," he said. "Or it could be that they moved away out of state without notifying DHS. Or it could be that they simply don't want to be part of the workforce. They're able-bodied, but ... they don't desire to do it."
To Ruelle, though, losing health coverage only makes it harder to participate in the workforce.
"When I work, I stand, you know? I stand on my feet for hours a day," she said. "I don't like taking medicine, period, but facts are facts: I need to be out of pain in order to work. I can't work if I can't even move." Her asthma, meanwhile, gets worse when the weather turns cold; she starts wheezing when she goes without the Advair inhaler for too long, she said.
Ruelle signed up for Arkansas Works insurance soon after she was released from prison in January 2017. She'd been serving time for a drug offense. "I went to prison over bad choices in my life. I got mixed up with the wrong crowd, got into using narcotics and drinking heavily and stuff like that, and I paid the price for it," she said.
Now, Ruelle said, she's four years sober and determined to stay that way. "I'm really trying, I really am. I work a 12-step program. I have sponsees [people she sponsors]. And I don't mess up, because I don't need them looking at me and saying, 'Oh, it's OK to mess up and stuff.' ... No, I'm trying to save my life. I'm doing the things I need to do in order to keep my life stable." Originally from the Pine Bluff area, she's now intent on starting fresh in a new town. "I'm trying to set a foundation here in Little Rock," she said.
But she's worried about what happens when her prescriptions run out. "I mean, I've thought about this, and it's steadily going off in my brain. I'm having to function with a smile on my face in pain, but I do it. Don't get me wrong, I love my job. ... I love my customers, I love making them smile, and I get to do that. It's part of my job, customer courtesy, and when you're in pain, it's really hard to smile. It really is."
Ruelle's job offers health insurance to supervisors but not to lower-level staff, she said. She's talked to an independent insurance agent who's arranged for her to get insurance on Jan. 1, either by re-enrolling in Arkansas Works or by enrolling in the health insurance marketplace, where she would pay a small premium. Until then, she'll keep working as best she can.
"I mean, I gotta pay bills, so I work," she said. "I have to pay rent."
Disconnected, disenrolled
Most people on Arkansas Works were likely working long before the state's requirement came along. An analysis released last December by the Kaiser Family Foundation, a national health policy research nonprofit, found that about 60 percent of working-age, able-bodied adults on Medicaid worked full time or part time. Most of those in the remaining 40 percent said they were in school, retired, taking care of a family member or too ill or disabled to work — situations that would likely make someone eligible for an exemption under Arkansas's rules.
But DHS numbers show that among people required to report work activities last month, only about one in nine complied.
In October, the work requirement applied to 69,041 people, according to the most recent DHS report. The vast majority, 55,388, did not have to report anything, either because they received an exemption or because the department had income information on file that made the agency assume they were working enough hours. (The fact that many workers are automatically deemed exempt from reporting may add to confusion about who exactly is required to report.) Just 1,525, or about 2 percent of the total, satisfied the rule by actually logging on to DHS website and reporting 80 hours of work activities. That left 12,128 people who didn't meet the reporting requirement that month. Of those, 3,815 had reached their third month of noncompliance and had their cases closed.
National health policy advocates have expressed alarm over such figures. On Nov. 8, the Medicaid and CHIP Payment and Access Commission (MACPAC), a nonpartisan federal advisory panel, sent a letter to Medicaid officials in the Trump administration calling for a "pause in disenrollments" in Arkansas. The fact that so few people were reporting work hours suggested the policy "may not be structured in a way that provides individuals an opportunity to succeed, with high stakes for beneficiaries who fail," commission chair Penny Thompson wrote.
One way to interpret the low reporting rate is that many beneficiaries aren't motivated to keep their insurance. Another is that many people, such as Ruelle, simply aren't sure what they're supposed to do.
Robert Smith, 48, got a letter in late October telling him he'd be cut off on the first of the month. "They said I hadn't completed my 80 hours. I didn't even know I was supposed to complete 80 hours," he said in a recent interview.
Smith, who lives in Benton, said he's now only able to work intermittently because of chronic back problems and a torn rotator cuff. He currently works part time hauling trash, despite the pain in his back and shoulder. "It's pretty tough. You just gotta bear it and do what you gotta do," he said.
Smith has also been diagnosed with abnormally low testosterone levels, he said, and for the past 17 years has received regular injections of the hormone from a doctor. Arkansas Works covered those injections. The insurance wasn't perfect — it didn't cover his X-rays after a recent fall, he said — but he's not happy about losing it over a requirement he only just heard about.
"I didn't even know nothing about it until it was too late. And, I mean, how are you supposed to work if your back's messed up? Do I have to go and volunteer 80 hours somewhere? I don't understand what they're wanting," Smith said.
To policymakers who might ask why he was only holding down a part-time cash job, Smith said he'd point out to them that he worked hard for decades.
"You know, my kids are raised. I don't owe nobody, nobody owes me nothing, so I took the last year and a half off just for me," Smith said. "Because I've been killing myself all my life." Still, he said, "I have no problem taking a job that I'm capable of doing without tearing my shoulder or messing my back up more."
In its Nov. 8 letter, the federal commission criticized Arkansas's insistence that beneficiaries use the web portal to report hours, considering the state has one of the lowest levels of internet connectivity in the nation. (Census data compiled by the Urban Institute, a D.C.-based think tank, show about 18 percent of households lacked home internet access in 2016, including no access through a cell phone.) Yet DHS has made many of its educational resources available only online or through social media, the letter noted.
DHS Director Cindy Gillespie has said the web portal is a means of pushing beneficiaries to gain computer literacy skills. "We need to help them get an email [address] and learn how to deal in that world, or they will never be successful," she said in March. However, DHS has devoted no additional resources to teaching beneficiaries those skills. Gillespie also acknowledged at the time that online-only reporting would help the agency save money. "If you implement it in the old-fashioned way of, 'Come into our county office,' we would have to hire so many people," she said.

DHS insists it's doing everything it can to keep people informed. It contracts with the Arkansas Foundation for Medical Care to operate a call center. It regularly sends mail to beneficiaries informing them of their status (perhaps to excess — many complain of receiving a torrent of redundant and often contradictory letters from DHS). It has established a "registered reporter" process, which allows third parties to relay information from beneficiaries who have trouble reporting through the web portal.
Most registered reporters are insurance brokers, agents or others affiliated with the private insurance world. Insurance carriers have an incentive to keep Arkansas Works beneficiaries enrolled because of Arkansas's unique public-private approach to Medicaid expansion, in which the government pays for the cost of private insurance for most beneficiaries. The plans are provided by the state's three health insurance marketplace carriers: Arkansas Blue Cross Blue Shield, Ambetter of Arkansas and QualChoice. (Both Ruelle and Smith were enrolled in Blue Cross plans.) In other words, when beneficiaries get kicked off Arkansas Works, the companies stand to lose money.
Max Greenwood, a spokeswoman for Arkansas Blue Cross Blue Shield, the state's largest carrier, wrote in an email that the carrier has designated "close to 200" employees as registered reporters. "We have made close to 10,000 telephone calls, sent approximately 115,000 letters, approximately 10,000 texts and about 27,000 emails in hopes of reaching impacted members," she added. Blue Cross has also reached out to providers and pharmacists to offer their patients assistance with reporting.
Still, Blue Cross has seen 6,857 members disenrolled due to the work requirement as of Nov. 15, Greenwood said. She said it's "fair to say that there is still a significant number [of beneficiaries] that are unaware they are subject to the requirement."
A spokesperson for Ambetter, the second-largest carrier in the state, said by email it had also "implemented a robust outreach plan for both members and providers." Ambetter has had 4,259 members disenrolled because of the work requirement as of Nov. 13. The spokesperson added that "members report that internet access, computer literacy and lack of transportation are their greatest challenges to meeting the work requirement."
It's unclear how effective these outreach efforts have been. The Medicaid commission letter noted that DHS was unable to provide data on how many beneficiaries had been helped by registered reporters.
Holes in the system
Even some beneficiaries who are well equipped to navigate the work requirement say it has disrupted their lives.
Kadie Campbell, 38, is a resident of rural Washington County and a graduate student at the University of Arkansas; she's on track to receive a master's degree in clinical mental health counseling at the end of this semester. She's been on Arkansas Works for a couple of years, she said, and until October she was enrolled in a Blue Cross plan.
Campbell is considered a "full-time equivalent" student by the university. DHS says full-time students are exempt from the work requirement. But Campbell soon found she isn't considered "full-time" by DHS, because she only spends three credit hours each week in a classroom. Her final semester of grad school is spent mostly in the field: She interns at a women's prison, which she visits three days a week to conduct interviews with inmates, typically for five to six hours each day. She usually spends another 15-20 hours per week at home, reviewing videos from her interviews, doing paperwork and studying. She has to log at least 300 hours over the course of the semester, she said.

When DHS notified Campbell she'd have to begin meeting the work requirement in July, she first tried to claim the student exemption. "I put in that I'm full time — and for graduate students, this is full time — but their system doesn't recognize that," she said in a recent interview. "There's not a distinction between undergrad and graduate work."
So, she pieced together a plan. DHS counts every college credit hour for 2.5 "work activity hours," meaning the three-hour class would give Campbell just 7.5 hours each week to count toward the work requirement. "I talked to my adviser and the professor, and we decided that the hours spent in the prison can be counted as volunteer work, but the hours I spend outside the prison doesn't count for anything," she said. (Each volunteer hour equals one "work activity hour" in the system.)
Manley, DHS spokeswoman, said a grad student's internship hours would likely have to be entered in a separate education category. Such time might be considered "occupational training," which comes with its own time multiplier. Campbell said she didn't realize that was an option. She was simply following the rules regarding "college and university" hours on DHS materials.
Over the summer, Campbell picked up a part-time job at the Fayetteville Public Library working 16-20 hours per week. That wasn't initially because of the work rule, she said; she needed the money. But she decided to keep working eight hours a week at the library even after the semester began, just to make sure she met the monthly requirement.
Though she found the work rules frustrating, Campbell studied them carefully. She knew she'd lose her insurance only after three months of noncompliance. She wouldn't reach the requisite 80 hours per month in July or August, but she figured she'd be fine once the semester began.
"It was, I think, Sept. 28 that I got a notice from Blue Cross Blue Shield that my insurance was taken from me," Campbell said. She was shocked. She'd been told she had until Oct. 5 to report her hours for September and had been waiting until she got her check from the library at the end of the month.
She called Blue Cross, which confirmed her insurance had been turned off due to the work requirement. She called DHS, which told her to call her county office. She called the Washington County DHS, which referred her back to the state. Eventually, she spoke to a supervisor in Little Rock who looked at her information and confirmed she only had two months of noncompliance and should not have lost coverage.
"She said it's set up automatically so that if you haven't entered anything by the 27th or 28th ... the system automatically kicks you out," Campbell recalled. "She just kept saying, 'The system is new, and we're trying to work out kinks, and there are people with problems.' "
The DHS employee told Campbell she could immediately re-enroll but that she'd initially be covered through fee-for-service Medicaid, rather than Blue Cross.
"And I'm like, well, that's great, but my mental health counselor doesn't take Medicaid," Campbell said. She was told she should be able to re-enroll in Blue Cross in December or January. Until then, her counselor has agreed to see her pro bono, which she's thankful for. ("As a clinical mental health graduate student interning at a women's prison, it's pretty important that I have my own counseling," she added.)
Manley said the work requirement shouldn't trigger a closure before the last day of the month. Asked by email whether beneficiaries have been accidentally disenrolled after only two months of noncompliance with the work requirement, she replied that "no known instances of this have occurred." However, Campbell provided a screenshot of the Access Arkansas portal showing that she'd been noncompliant for just two months as of November, along with letters from Blue Cross notifying her that her plan would be closed at the end of September.
"I really don't understand why things happened. I just know that they did," Campbell said. "I think that it's messed up and it's wrong and my coverage was taken from me unfairly. I have met every requirement and I have actually gone above and beyond."
She also wonders if other low-income Arkansans are falling through the cracks. "I have the luxury of being able sit around on the phone for as long as it takes to get ahold of somebody — and being eloquent enough to explain my situation," Campbell said. "I'm savvy with a computer system. I'm working diligently to become a productive member of society. ... If I'm getting screwed, then how many other people are?"
Others losing coverage
The Arkansas Works program was shrinking well before the work requirement. Enrollment on Jan. 1 was 286,000. By Nov. 1, it had slipped to 246,000. Of the 40,000 who left Arkansas Works over that 10-month span, only about 12,000 cases were closed due to the work requirement, leaving 26,000 whose coverage ended for other reasons.
Governor Hutchinson has attributed the reduction to a strengthening economy and improved efforts at DHS to scrub the rolls of those no longer eligible for Arkansas Works. That group include workers making too much money to qualify for the program — for a one-person household, the monthly income threshold is $1,397 — along with people who have moved out of state, inmates at correctional facilities and seniors who have become eligible for Medicare. But it also includes cases closed for what might be called technical compliance issues, such as not responding to a DHS request for information quickly enough.
Two people interviewed for this story thought they had lost coverage due to the work requirement, but an inspection of letters sent from DHS revealed they'd been cut off because of a missing paperwork issue. DHS said it could not comment on individual cases, but its most recent report showed that almost 4,200 cases were closed in October alone because the beneficiary "failed to return requested information." (People whose cases were closed for reasons other than the work requirement are not subject to the lockout period and may re-apply for coverage. However, if people think they were kicked off due to the work requirement, they may also assume they're locked out.)
Kevin De Liban, an attorney for Legal Aid of Arkansas, is among the lawyers representing nine plaintiffs in the federal lawsuit seeking to undo the state's work requirement. (The National Health Law Program and the Southern Poverty Law Center are also working on the suit.) DeLiban said Legal Aid has seen an increase in people kicked off for failing to provide DHS with verification of income or other household information within 10 days of receiving notice, as the agency requires.
"In many cases they did, it just wasn't processed in time. Or maybe they provided it on day 11 or 12, but their case was already set to be closed," De Liban said. "It's immensely confusing, because it's more and more administrative hoops to jump through and figure out. ... Some people might have reported [work hours], or might not have, but then they get kicked off in the meantime for something other than the [work] requirement.
"And so it's, if they don't get you through the work requirements, they might get you through the verification procedures or the returned mail," he said. "At least from our clients' perspective, it seems like the state is trying to make it as hard as possible for people to retain coverage."
The cost of labor
In September, when the work requirement first began locking people out of coverage, Hutchinson said cutting off beneficiaries was not the policy's goal. "We'd like to see them all in compliance," he said at the time.
The governor noted that he's long defended Medicaid expansion from fellow Republicans in the state legislature who want to dismantle the program entirely. "I fought hard to maintain Arkansas Works, despite odds against it, despite enormous criticism," Hutchinson said. The work requirement represents a "proper balance," he said, between "providing assistance to those who need it, and ... the value of work and responsibility."
Hutchinson cited data showing many Arkansas Works enrollees had recently found employment, some of them assisted by the state Department of Workforce Services. At dozens of workforce centers around the state, DWS staff help clients search for jobs, prepare resumes, obtain scholarships and more.
Out of 21,841 Arkansas Works beneficiaries referred to DWS due to the work requirement, 1,366 have sought help at a workforce center as of Nov. 14, DWS spokesman Steve Guntharp said in an email. Some 2,887 people subject to the work requirement have found full-time employment since the requirement started. (That's with or without DWS assistance; the number was derived from the state's New Hire Registry, Guntharp explained.)

It's not clear what job gains can be attributed to the work requirement, because the working poor commonly cycle in and out of employment. Guntharp said DWS doesn't ask clients whether the requirement motivated them to seek work or whether they were looking for a job anyway. Workforce centers haven't seen a major rise in casework recently, he confirmed, and DWS hasn't hired additional staff.
In its Nov. 8 letter calling for a pause in disenrollments, the Medicaid commission criticized Arkansas for not collecting better information on whether the state's work supports are meeting people's needs. "[D]ata currently are not being reported on the extent to which beneficiaries are accessing such services, what services they are asking or qualified for, which barriers may exist for their use of these services, and whether services are being delivered," the letter said.
The Department of Workforce Services would not allow a reporter access to a workforce center to interview clients or staff, citing privacy concerns. When asked to be connected with Arkansas Works success stories, the agency emailed profiles of two individuals, Julia Bunch of Harrison and Jeff Snyder of Rogers, along with signed consent forms.
Snyder's profile said he sought help from the Rogers Workforce Center after being unemployed for nine months and searching unsuccessfully for jobs. With the help of a workforce specialist, Snyder, who had recently earned his associate's degree, found a new job Aug. 8 making $17.64 an hour. "I now work with a great company — in a job that I actually would not have gotten without the help from DWS," he was quoted as saying.
The profile did not say whether Snyder reported being motivated by the work requirement. Moreover, this reporter could not independently confirm the details provided by DWS. The agency said it could not provide contact information for Snyder or Bunch because of confidentiality laws. Other attempts to contact either beneficiary for an interview were not successful.
Whether motivated by the work requirement or not, some beneficiaries are undoubtedly finding better-paying jobs, considering the strong economy. But not all jobs come with insurance, and making more money often means losing eligibility for Arkansas Works.
Joe Thompson, the CEO of the Arkansas Center for Health Improvement, a nonpartisan health policy center in Little Rock, said any measurement of the work requirement must take into account both income and health outcomes. "It's not just getting a better job. ... It's a two-step process," he said. "You want [the beneficiary] to get a better job that has insurance or buy insurance on the individual marketplace. So success needs to be not just, 'Are they working?' but, 'Are they being successful in moving up that socioeconomic ladder and maintaining health insurance coverage?' "
Arkansas Works beneficiaries interviewed for this story — including some not mentioned by name above — expressed mixed feelings about the concept of a work requirement. A few said they felt it was a good idea in principle but believed the state was executing it poorly. All complained that the online-only reporting mechanism was flawed.
Many, like Nannette Ruelle, expressed anger and indignation that Arkansas was rescinding health coverage for its poorest citizens, many of whom depend on it for their day-to-day health needs.
"This was put in place to help us, and it helped us for like a short period of time, and then it was like ... whoever the caseworker is didn't do their part," Ruelle said. "They're getting paid to do their job, but they're not even doing it."
Dealing with DHS, she said, makes one feel "like you're just a number on a sheet of paper. That's exactly how they treat you." It fills her with the same sense of powerlessness she had when she was incarcerated. "If that were the case, why didn't I just stay in prison?
"I served my time, and I'm ... a resident of the United States of America, Little Rock, Arkansas," Ruelle said. "I'm a resident here, and I pay my taxes, which helps pay them, so I would expect something in return. I'm paying you, so I need some help back."
This reporting is made possible in part by a yearlong fellowship sponsored by the Association of Health Care Journalists and supported by The Commonwealth Fund. It is published here courtesy of the Arkansas Nonprofit News Network, an independent, nonpartisan project dedicated to producing journalism that matters to Arkansans. Find out more at arknews.org.
