When Arkansas expanded Medicaid in 2014, Mike Haynes signed up for health insurance for the first time in his adult life. "Before that, I really couldn't afford it," he said. "One income in the state of Arkansas is very tough when you're raising two children. I did it, but I couldn't afford fringe benefits, so to speak. I had to feed my kids and put clothes on them."
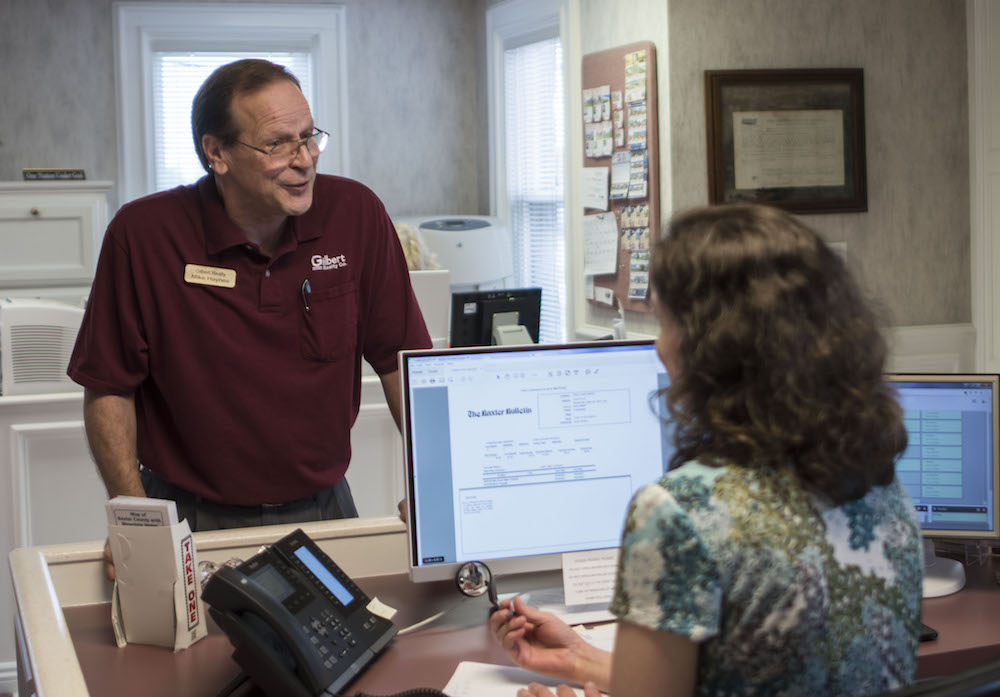
Haynes, 63, is a real estate agent in Mountain Home. His children are grown now, but things remain tight. "We're eating bologna, not steak," he said. His wife has multiple sclerosis and can no longer work (she qualifies for the traditional Medicaid program through her disability benefits), and Haynes' income fluctuates dramatically with the housing market. In 2014, "paychecks were few and far between," he said, and he signed up for coverage under the state's Medicaid expansion, which offers coverage to Arkansans who make less than 138 percent of the federal poverty level (that's $16,400 for an individual or $33,600 for a family of four).
A year later, his wife encouraged him to go in for a routine physical, and he ended up being diagnosed with prostate cancer and Hodgkin's lymphoma. "It was an eye-opener, extremely scary," Haynes said. "All of a sudden your whole world changes."
The doctor told him that if he hadn't come in, he had two years left to live. Now, he's in remission after a dozen sessions of chemotherapy. "I can't stress enough how much it meant to me to have coverage," Haynes said. "I knew I wasn't going to lose my house and everything else." Before getting coverage, Haynes had always avoided going to the doctor because he assumed he wouldn't be able to pay the medical bills, and he said he would never have gone in the first place without health insurance.
"Two things saved my life: Obamacare and my wife," Haynes said. "That's the truth."
Haynes has been able to get his treatment at Mountain Home's Baxter Regional Medical Center, recently named one of the top 100 rural and community hospitals in the nation by the National Rural Health Association.
The Medicaid expansion has been just as vital to Arkansas's rural hospitals as it has been to patients like Haynes, said Ron Peterson, Baxter Regional's CEO. The reduction in uncompensated care has led to a $4.2 million annual positive impact for the hospital, Peterson said. "The expansion meant the difference between us running in the red vs. running in the black," he said.
Arkansas is one of 31 states — few in the South — that expanded Medicaid eligibility to low-income adults like Haynes as part of the Affordable Care Act. The state used a unique approach known as the private option — later rebranded "Arkansas Works" — which uses Medicaid funds to purchase private health insurance for the newly eligible population. The federal government pays for most of the costs through funds made available by the ACA.

The ACA's crafters essentially made a deal with hospitals: The ACA cut Medicare reimbursements, but the reduction in uncompensated care through the Medicaid expansion helped offset some of those cuts. Without that offsetting boost, some of the state's smaller rural hospitals might not be able to survive. A hospital like Baxter — the fifth most Medicare-reliant hospital in the nation, according to Moody's, thanks to the community's significant proportion of retirees — would be forced to make dramatic cuts in services without the Medicaid offset. "The expansion of Medicaid through Arkansas Works is one of the key components that's been able to help us through the change in the ACA," Peterson said. "Not just Baxter, but it helps all of rural Arkansas."
The political future of the Medicaid expansion, however, remains dicey. State Sen. Scott Flippo, a Republican who represents the area, campaigned on ending the program and has voted multiple times for unsuccessful attempts to defund it in the Arkansas legislature. Meanwhile, the American Health Care Act, the bill backed by President Trump and passed by the U.S. House of Representatives earlier this month, would end the ACA's enhanced funding for new and returning enrollees beginning in 2020, effectively ending the Medicaid expansion program. Trump won Baxter County with 74 percent of the vote.
Peterson said that he was hopeful that the AHCA proposal would be amended further, but as it stands, the phase-out of the Medicaid expansion "would be devastating to our hospital, and I think it would be extremely bad news for all rural hospitals."
It can be a challenge to explain the value of Medicaid expansion amid the always thorny politics of the national health care debate, Peterson said. "I think that people in Mountain Home really appreciate the hospital and appreciate the services that are provided here," he said, pointing to significant giving from the community to the Baxter Regional Hospital Foundation and the more than 500 volunteers who give more than 80,000 hours of their time every year. "They want to see this hospital succeed. I just don't think they see the tie and the connection with the Medicaid expansion."

Baxter Regional is by far the largest employer in the community, employing 1,600 individuals; its payroll is more than $70 million. Outside of the hospital, opportunities for professionals are few and far between, Dan Greer, a network analyst at Baxter Regional, said. Greer has worked at Baxter Regional for nine years; before that, he worked at the Baxter Bulletin, but lost that job after the newspaper was downsized. "If it wasn't for the hospital being here, I would have been gone," he said.
If the Medicaid expansion ended, Peterson said, "You're looking at easily 200-300 jobs eliminated out of the community. That may not sound dramatic, but it's dramatic in a community of our size."
Baxter Regional's mission is to remain independent and as comprehensive as possible, Peterson said, both of which would also be threatened if the hospital took a financial hit from the elimination of Medicaid expansion. "We believe that having that local input and that local control helps us be more community-driven and make sure we're meeting the needs of the community," he said. "And we try to provide urban medicine in a rural setting. Just because you live in a rural area should not mean you should not have access to quality care."
Baxter Regional offers cardiac surgery, comprehensive oncology services and 30 different specialties; this summer, the hospital will start offering neurosurgery. As a Level III trauma center, the hospital has the resources to provide care for most traumatic injuries.
"You can't measure the value on that," said Dr. Brad Shultz, a physician in the emergency room, where the hospital sees 30,000 patients a year. "The sick, aged population we have, if we didn't have the specialists, we couldn't buy enough ambulances to keep them all transferred."
That transport itself can be a dangerous part of medical care. "Every time they're exposed to a new health care setting, it's adding risk to their situation," Gerald Cantrell, the hospital's paramedic director, said. In nonemergency situations, meanwhile, a multiple-hour drive may discourage patients from seeking the care they need.
"We're fairly isolated," Peterson said. "The next hospital that has all the types of services that we have is at least two hours away."
The hospital has invested in technology to deliver high-quality care to its isolated community. In its intensive care unit, the hospital has an "electronic ICU" that provides 24-7 access to intensive care specialists in St. Louis. Its radiology department was one of the first in the state to use 3D tomosynthesis for mammography, which is more accurate and leads to fewer call backs, and the first in the nation to develop a mobile 3D tomosynthesis unit in a custom-made RV that offers screenings in the community. "It allows us to take the mammography out to where the patient is, and helps us get to even more remote areas than Mountain Home," Peterson said. "We're going to the rural community and bringing that technology to them."
The STEMI program (STEMI is the medical shorthand for a severe heart attack) has a coordinated system in place to communicate between paramedics and the hospital to deliver care as quickly as possible — and crucially, Baxter Regional has the cath labs (diagnostic imaging equipment necessary for the optimal treatment of a heart attack) and specialists to provide an immediate intervention.
"A lot of your smaller rural hospitals won't have cath labs," Peterson said; they can offer only less effective clot-busting drugs. "If we weren't the size hospital that we are and started cutting back, you could see people having a heart attack, getting a drug, and being shipped off and not getting that intervention for three to five hours when they need to be getting it right away."
"Arkansas has the highest mortality rates nationwide for death from heart attack," Dr. Kim Foxworthy, the STEMI coordinator, said. "Our statewide mortality rates would definitely be higher if we did not have the technology and facility here. People are just not going to make it."
Just as important, Peterson said, was the hospital's commitment to outreach. He cited the community paramedic program, which offers direct services to high-needs patients in their homes, and four on-site Community Health Education and Support Houses, which offer services for patients and their families for diabetes, cancer, aging and women's health.
Without the Medicaid expansion, Peterson said, the hospital would be forced to make difficult — and potentially life-threatening — choices about what services to cut. That would impact everyone who relies on Baxter Regional, not just those covered by the Medicaid expansion. Servicing a remote community in the Ozarks with a population that isn't growing, it's unclear how the hospital would make up the funding gap if expansion goes away.
"The numbers do not add up," Peterson said. "Unless you want to abandon people who live in rural America."
Haynes, the cancer survivor who got coverage thanks to the Medicaid expansion, said he remembers years ago having to drive more than two hours to Springfield, Mo., to get to a hospital with an incubator when his daughter was born. "That's a thing of the past," he said. "I received outstanding care here. It's a tremendous service to the community."
Haynes voted in the presidential race for the first time last November and, like most of his neighbors, he voted for Trump. "I felt like we were going to be in the same position no matter what Hillary did, we needed some improvements, and I really just wanted a guy that wasn't involved in politics," Haynes said. He said he has been watching the progress of the AHCA with concern, particularly when the Congressional Budget Office found in March that an earlier version of the bill would lead to 24 million fewer people being covered (the CBO released a new score for the amended version of the AHCA on May 24, finding that 23 million fewer would be covered).
"I guess I was naive because when he spoke 'change,' in my mind, I thought 'even better,' " he said. "And then as it moved along and 24 million people weren't going to get coverage, I thought, 'What's going on? Am I one of the 24 million?' "
After he wasn't able to work for a year and half because of the cancer, Haynes has just started back at his job. "It'll get better — the economy is getting better, I'm getting better, so I'm very positive about the future," he said.
Haynes said he's still grateful for President Obama. "I'd vote for the man tomorrow," Haynes said. "I don't play politics. But the man did a lot for me, period. Without Obamacare, I wouldn't be sitting here. How would you feel?"
This story was supported by the nonprofit Economic Hardship Reporting Project, part of an initiative to foster journalism about inequality in the South and the Heartland, and is also courtesy of the Arkansas Nonprofit News Network, an independent, nonpartisan news project dedicated to producing journalism that matters to Arkansans.