
On June 1, with the blessing of the Trump administration, Arkansas became the first state in the 50-year history of the Medicaid program to impose a work requirement on certain beneficiaries.
Medicaid provides publicly funded health insurance to almost 1 million Arkansans — including the disabled, the elderly and children on ARKids — but the new work requirement will apply only to nondisabled, working-age, low-income adults. Around 280,000 such beneficiaries are covered by Arkansas Works, the state's name for Medicaid expansion under the Affordable Care Act. (Somewhat confusingly, the program has been called "Arkansas Works" since 2015, though the work requirement itself is a new feature.)
At first glance, the requirement is both limited in application and modest in scope. Even among Arkansas Works beneficiaries, about 75 percent will be exempt. For the approximately 69,000 recipients to whom the requirement may apply, the state Department of Human Services will mandate 80 hours of approved "work activities" each month, which can include school, job searches and volunteering along with punching the clock. Governor Hutchinson, who championed the policy, has cited Arkansas's 3.8 percent unemployment rate as evidence it's reasonable to ask able-bodied adults to find a job.
"This is not about punishing anyone," Hutchinson said March 6, when the federal Centers for Medicare and Medicaid Services (CMS) approved Arkansas's waiver implementing the requirement. "It's to help them to move out of poverty and up the economic ladder." Asked how many people were likely to lose coverage, Hutchinson said he expected noncompliance to be "minimal."
Yet health care advocates warn that Arkansas's experiment could nonetheless lead to thousands losing insurance, including many who are now working.
One reason is that documenting the work activities of some 69,000 people each month will entail a dense new web of red tape. It's not enough to simply have a job; beneficiaries must report their work habits monthly through an online portal set up by DHS. Reporting by mail or phone will not be allowed — though the website may be unavailable up to 10 hours every day.
Any change of job that involves a change of income must be reported to DHS. Cash income, whether earned through mowing lawns or waiting tables, must be rigorously documented and reported. Though some exemptions are automatic, others must be reported regularly. And, if a beneficiary fails to report his or her information for three nonconsecutive months out of the calendar year, that person will not only be removed from the Medicaid rolls, but also be locked out of the program until the following January — regardless of whether he or she qualifies for an exemption later in the year.
Joan Alker, the executive director of Georgetown University's Center for Children and Families, has been closely tracking the progress of work requirements in Arkansas and elsewhere. "I think the lessons of history are very clear," she said. "When you have more red tape and paperwork, people lose coverage. When you have more uninsured parents, you're probably going to see more uninsured children as well."
"We're extremely concerned about significant losses of coverage as a result of these new requirements being rolled out in a very rushed manner," she said.
Hospitals are also concerned. Coverage losses would lead to more uninsured people using emergency rooms for care, driving up costs and threatening small hospitals' survival.
"If someone who is eligible for the program loses their eligibility ... their care through the hospital now goes to uncompensated care," Arkansas Hospital Association President and CEO Bo Ryall said. (The AHA is a donor to the Arkansas Nonprofit News Network, sponsor of this article.)
Our House, a shelter for the working homeless in Little Rock, is one of dozens of employment and training (E&T) sites statewide that assist beneficiaries on the food stamp program, or SNAP. Lyndsey Czapansky, who runs the E&T program at Our House's career center, said staff are actively training to help clients navigate the system. Still, she's concerned about the possibility of clients losing coverage because of how it could affect their ability to find and keep employment.
"You need to be in good health to keep a steady job," Czapansky said. "When my clients come in, the first thing that we do is enroll them in Medicaid. If they're locked out, I don't know what we'll do, especially if they need mental health care or intensive dental work or diabetes treatment."
Marquita Little, the health policy director for Arkansas Advocates for Children and Families, said most beneficiaries probably are unaware of their new obligations. "Even the people who know about [the work requirement] don't know that they have to take action or what they need to do," Little said. "There are going to be a lot of opportunities for people to fall through the cracks."
***
Medicaid expansion has transformed health coverage in Arkansas since it was first authorized by the state in 2013. U.S. Census Bureau data shows Arkansas's overall uninsured rate fell from 16 percent in 2013 to 8 percent in 2016. Only Kentucky, a similarly poor state that also expanded Medicaid, saw a greater decline in its rate of uninsured adults over that period.
In 2015, when Hutchinson inherited Medicaid expansion from his Democratic predecessor, Mike Beebe, he chose to embrace the program. That angered some conservatives in the state legislature who have attempted each year to block the Arkansas Works budget in defiance of the governor. The reauthorization fight has replayed every year at the Capitol, pitting Republican against Republican.
But work requirements tend to unite the party. Days after Hutchinson announced the Trump administration had approved Arkansas's waiver, the GOP-dominated legislature passed the Arkansas Works budget with little fuss. Polls show work requirements are also broadly popular among the public: In a poll released last June by the Kaiser Family Foundation, a health advocacy group, about 70 percent of respondents said states should be allowed to implement such policies.
The majority of people on Arkansas Works likely already have jobs. A national Kaiser Family Foundation analysis released in December found that 42 percent of non-elderly Medicaid adults worked full-time and another 18 percent worked part-time, based on Bureau of Labor Statistics data. Among the 40 percent without a job at the time of the survey, about one-third said they weren't working because they were taking care of a family member and another third said they were ill or disabled. Most of the remainder said they were retired or attending school.
However, employment often comes in fits and starts for the working poor. A study published in May by the Urban Institute, a Washington, D.C., think tank, found that among those Arkansas Works beneficiaries who today hold a job, almost one-third may fail to meet the state's new requirements year-round. Of those low-income, employed beneficiaries who likely do not qualify for an exemption, 32 percent wouldn't meet the 80-hour threshold for at least one month out of the year.
Anuj Gangopadhyaya, the lead author of the Urban Institute study, explained that beneficiaries who "work in high turnover occupations or jobs with high seasonality could have their coverage jeopardized."
Census Bureau data indicates that when such individuals are working, they work far more than 80 hours per month, Gangopadhyaya added. "We found they're averaging about 35 hours per week, so it's not that they're opting to not work. ... It's more a matter of whether they have consistent work or not." DHS has said it won't allow beneficiaries to apply "surplus" hours accrued one month to later months that same year.
To supporters of the work requirements, such details are outweighed by a need to create accountability for Arkansas Works beneficiaries.
"I think that there are people who need some sort of encouragement to get job training or to accept the job," state Sen. Jim Hendren (R-Gravette), the GOP majority leader and a nephew of the governor, said in a recent interview. "I am a believer that deadlines work. ... I'm hopeful that by setting expectations, people who are getting some benefits of insurance by others paying for it realize that it's fair and reasonable that they should pursue and obtain work, so that they can contribute to the next person."
Beneficiaries subject to the requirement will be referred to the Department of Workforce Services, which is tasked with connecting those individuals to job training and wraparound services. However, the state has budgeted no new money for an influx of clients at its workforce centers. Hendren said he didn't think that would be a problem.
"If we get to the point where people are sincerely trying to get job training and the programs are not available, we either need to do a better job of making those programs available or we need to give them some relief on taking away their health insurance," he said. "I don't want to penalize people because we're asking them to do something impossible — but I don't believe right now that's the case."
***
Hendren also pointed out the exemptions are generously drawn. "I think there was a very fair and reasonable effort to make this apply to a population that really should be seeking employment and accepting it if it's offered to them," he said.
"Arkansas actually has quite broad exemption criteria compared to other states trying to implement work requirements," Gangopadhyaya acknowledged. Kentucky, Indiana and New Hampshire have also received approval from the Trump administration to impose work requirements, though Arkansas will be the first to get its system off the ground. (Based on estimates from Kentucky, about 40 percent of the 480,000 adults in that state who rely on Medicaid expansion are expected to be subject to the requirement, as opposed to about 25 percent of Arkansas Works beneficiaries.)
But a close examination of DHS' documentation reveals several surprising details about how the policy will actually operate. Contrary to what the governor has said, DHS will not require beneficiaries to work 80 hours per month. Instead, it will require they earn a certain level of income: $680 per month, which is the equivalent of working 80 hours at $8.50 per hour, Arkansas's minimum wage. Each month, Medicaid recipients will enter their earned income into the online portal, rather than the number of hours they have worked.
By using income as a proxy measurement for labor hours, DHS appears to assume all Arkansas Works beneficiaries are making minimum wage. Someone who makes twice that rate, or $17 per hour, would only have to work 40 hours each month to meet the $680 monthly threshold. A beneficiary fortunate enough to earn $34 per hour would meet the requirement by working just 20 hours each month, or five hours per week. In an email, DHS spokeswoman Amy Webb confirmed this accurately described its system for measuring work hours.
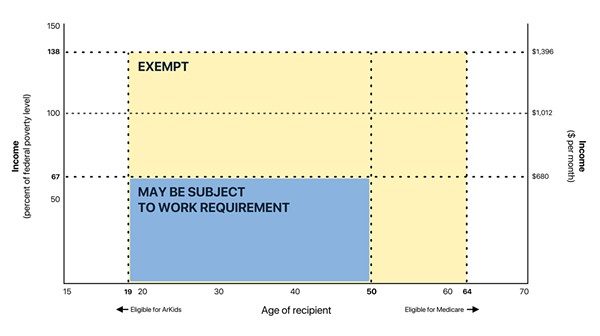
Arkansas Works covers low-income adults ages 19-64, but the requirement will apply only to those from ages 19-49. (It's being rolled out in phases: Those in the 30-49 age range must begin reporting in 2018 and those in the 19-29 range will begin in the first half of 2019.) People ages 50-64 are automatically and permanently exempt, meaning they will not have to report any information to DHS.
Perhaps more surprisingly, DHS will also automatically exempt anyone above a certain income level. DHS assumes beneficiaries who make more than $680 per month at the time they apply for health coverage are working enough hours to meet the requirement. That means the compliance burden of reporting work activities will only apply to people making below $680 per month, or about 67 percent of the federal poverty level. (To be eligible for Arkansas Works, a person must make less than 138 percent of the poverty level, or about $1,396 per month for an individual. Therefore, beneficiaries earning between 67 and 138 percent of the poverty line won't be subject to the requirement.)
Some exemption categories will require beneficiaries to report regularly to DHS: full-time student status, enrollment in a drug or alcohol treatment program, caring for an incapacitated person, "short-term incapacitation" resulting from a medical emergency, and a catchall "good cause" exemption that DHS staff must evaluate on a case-by-case basis. Webb said DHS workers will handle "good cause" exemption requests by phone or email.
Asked how much agency staff time would be required to assist beneficiaries and process exemption requests, Webb said the agency did not have an estimate.
Other exemptions will be automatically granted based on the beneficiary's initial application or other state data. Along with the age and income limits, these categories include workers receiving unemployment benefits, people designated "medically frail" due to certain diagnosed health issues, people already subject to a SNAP work exemption and women who were pregnant at the time of application.
Most importantly, an automatic exemption will also apply to anyone living in a household with a dependent child under age 18, whether or not the beneficiary actually cares for that child. That means a 25-year-old living with his parents would be automatically exempt from the work requirement if he has a minor sibling who lives at home. Marci Manley, a DHS spokeswoman, confirmed in an email that "any adult living in the home with a child under the age of 18 will have an exemption, they need not be a guardian or parent."
Little, the Arkansas Advocates policy director, said she was taken aback to learn the dependent child exemption was so broad. "I suppose as an advocate I should be saying 'Oh, that's great,' ... but the leakier it is, the more concerning it is that we are even rolling out this requirement," Little said. "If you have leaks on this end of it, you're going to have a lot of leaks in other places."
The exemptions are drawn so broadly that many likely won't be touched by the work requirement, Little acknowledged. "People that fall into their automated categories are probably going to be OK," she said. But workers on the margins of the economy who don't qualify automatically for an exemption may be in danger of losing coverage.
"I'm most worried about that group," Little said. "They're the people we see eligible for a couple months and then ineligible. They're the seasonal workers. They're people who inconsistently work because they can't get reliable permanent full-time employment. ... That's also where you're more likely to see people with mental illnesses or physical conditions where they're healthy one day and they're not the next."
***
The Center for Budget and Policy Priorities, a liberal-leaning D.C.-based think tank, warned the convoluted exemption categories would inevitably confuse beneficiaries. "These policies are so inherently complex that even if they try to put in exemptions and exceptions, they're still hard to implement and hard for people to take advantage of," Jennifer Wagner, a senior policy analyst with the CBPP, said in a recent conference call.
The confusion may be exacerbated by the fact that DHS, in an effort to minimize expenses, intends to administer the requirement without hiring any new employees.
"Arkansas has tried to do it in a way that hasn't increased staffing costs," Wagner said. In pursuit of a fully automated system, DHS expects all beneficiaries to report through the web portal, an unusual policy feature that required approval from federal CMS.
DHS Director Cindy Gillespie has said the online-only reporting requirement is an effort to save money. "If you implement it in the old-fashioned way of 'Come into our county office,' we would have to hire so many people," she said in March, soon after the waiver was approved.
Gillespie said the agency's long-term goal was to make all of its communications electronic. She also framed the portal as a means of pushing younger beneficiaries to gain computer literacy skills. "We need to help them get an email [address] and learn how to deal in that world, or they will never be successful," Gillespie said.
But the Urban Institute analysis of 2016 Census Bureau data found that among the 69,000 beneficiaries likely to be subject to the requirement, over a quarter had no internet service at home or regular cell phone service. Over half lacked broadband access. An online-only requirement, Gangopadhyaya said, is "a curious thing to do in Arkansas, which has the second-lowest internet access [rate] in the entire nation."
Little noted that DHS hasn't built a dedicated system to handle the complex new requirements. "It's the same Access Arkansas page that people have always used," she said. "We've kind of piecemealed the IT part of this. ... I think it would have cost more to build a system that was more user-friendly."
Alker, the Georgetown professor, pointed out DHS has had serious IT problems in the past. "Arkansas does not have a great history in terms of its eligibility and enrollment systems working well to begin with," she said. In 2015, tens of thousands of beneficiaries were kicked off of Medicaid due to changes in the state's income verification process — a mess that took months of work to resolve.
In a monitoring plan DHS submitted to federal CMS in May, the agency noted another detail: "The portal will be available daily between 7 a.m. and 9 p.m. except for times when it is necessary to take the portal offline for system upgrades." That suggests the system could be unavailable for up to 10 hours out of every day. Asked why the portal would be offline so often, Webb said by email that "this is the time when the system does updates, maintenance, and handles batch processing, etc."
Sen. Hendren admitted this part of the rollout could be rocky. "There's no question there may be some problems we'll have to solve in regards to people with limited internet access or those IT problems at DHS," he said. "But that does not mean you just do nothing and abandon the effort to continue to help people find employment and job training."
Computer systems may also help explain why Arkansas has kept its implementation costs much lower than that of Kentucky, which intends to begin implementing its work requirement in July. DHS says it has spent about $7.6 million on the work requirements this fiscal year. The figure includes $6.8 million spent on the IT system changes, 90 percent of which were paid by federal funds.
In contrast, the Louisville Courier-Journal reported in February that Kentucky increased its administrative budget for Medicaid by about $187 million for the fiscal year. Dustin Pugel, a policy analyst with the Kentucky Center for Economic Policy, a think tank in Berea, said most of that amount is expected to go toward IT contracts and workforce services administration.
"We already had an online application system and we just expanded that functionality to accommodate the reporting of activities," Webb wrote in an email when asked about the discrepancy in costs between the two states.
Like Arkansas, Kentucky is trying to avoid bringing on new staff to administer the requirement. "[Kentucky Gov.Matt Bevin] has said more than once they don't plan on hiring a single person to help administer this waiver," Pugel said. (Kentucky's work requirement is being challenged in federal court by a group of beneficiaries who say the Trump administration overstepped its legal authority when it approved the state's waiver, a case that could have ramifications for Arkansas.)
In Arkansas, the other $800,000 spent by DHS paid for a contract with the Arkansas Foundation for Medical Care to place phone calls to beneficiaries. DHS has also sent letters to enrollees and made a series of informational web videos. But informing 69,000 people of a complex new requirement will take a massive outreach effort, and DHS is expecting much of that task to fall to other outside parties: commercial insurance carriers.
In Arkansas, most Medicaid expansion beneficiaries are covered by private plans sold by insurers on the state's health insurance marketplace, rather than regular fee-for-service Medicaid. That unusual approach to expansion — dubbed "the private option" — means carriers have a financial stake in preventing the work requirement from eroding coverage gains.
Max Greenwood, a spokeswoman for Arkansas Blue Cross and Blue Shield, the largest carrier in the state, said the company is already contacting Arkansas Works members subject to the requirement. DHS will send each carrier a weekly list of their members who are exempt and those in danger of losing coverage.
"We've also reached out to all our agents, our brokers, our customer service teams, our provider partners and our retail stores to help provide additional support and direct member engagement," Greenwood said.
However, many beneficiaries rarely communicate with their insurance carrier. Providers such as hospitals typically won't be able to see when a patient is in danger of losing coverage.
"Hospitals will be helpful, and most hospitals do have Wi-Fi access or the ability to find someone a computer terminal," the AHA's Ryall said. "But, we don't have the in-depth information to identify someone who comes into the hospital and says, 'You need to enter this information.' Our people will certainly be asking those questions, but it will be up to the patient to let us know if they need assistance."
The requirement will indeed create much work — for beneficiaries logging their hours, for DHS staff vetting paperwork, and for insurers, providers and advocates helping thousands of enrollees navigate a new layer of bureaucracy. It is less clear whether the policy will lead to either significant gains in employment or reductions in coverage. But in the view of Hendren and other Republicans, the work requirement is a vital part of keeping Arkansas Works manageable.
"I want you to understand, the purpose is not to take away health insurance for people. The purpose is to make the program sustainable," Hendren said.
"We know we're always going to have people who get into a bind, and we certainly know that it helps to provide health care to folks in those situations," he added. "But we also know that there's no free lunch and money doesn't grow on trees, and we have to do our best to manage the program so that it doesn't become unsustainable and we have to make dramatic cuts."
This reporting is made possible in part by a yearlong fellowship sponsored by the Association of Health Care Journalists and supported by The Commonwealth Fund. It is published here courtesy of the Arkansas Nonprofit News Network, an independent, nonpartisan project dedicated to producing journalism that matters to Arkansans. Find out more at arknews.org.
