The cost of health insurance may feel unreasonably high, but everything’s relative: Data published on Nov. 1 showed Arkansas continues to see some of the lowest premiums in the U.S., both for employer-sponsored insurance and plans purchased on the individual marketplace.
Open enrollment for the 2019 individual marketplace began Nov. 1. A Kaiser Family Foundation analysis of average benchmark premiums on the marketplace showed the Arkansas rate was $378 per month for a 40-year-old individual — significantly lower than the national average of $477. The state’s 2019 average premium is a $14 increase over its average rate in 2018.
Most Arkansans who buy individual marketplace plans in 2019 will pay much less than $378 per month out of pocket, however. The Affordable Care Act created an income-based sliding scale of federal subsidies that help lower the cost of premiums for consumers. The benchmark rate is based on the cost of a premium for a “Silver” level plan; high-deductible “Bronze” plans are generally cheaper, while “Gold” tier plans are generally more expensive. (Consumers can find exact prices at http://healthcare.gov.)
Also on Nov. 1, the Arkansas Center for Health Improvement published an infographic showing Arkansas’s premiums for employer-sponsored insurance were the second-lowest in the country in 2017. The state had the lowest rates in the country from 2013 to 2016. Average premiums for employer-sponsored plans in 2017 were $5,722 for an individual and $16,663 for a family, the ACHI report said.
For the individual marketplace, premiums in Arkansas were also lower than in neighboring states, ACHI noted. The 2019 average benchmark premium was $444 in Texas, $454 in Louisiana and higher in other states bordering Arkansas. The figure in Oklahoma was $696, among the steepest in the country before a subsidy.
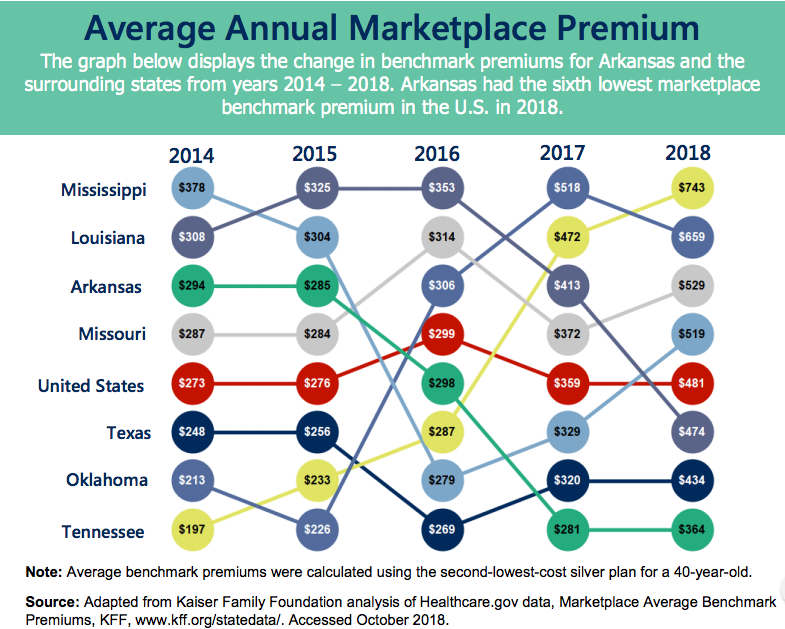
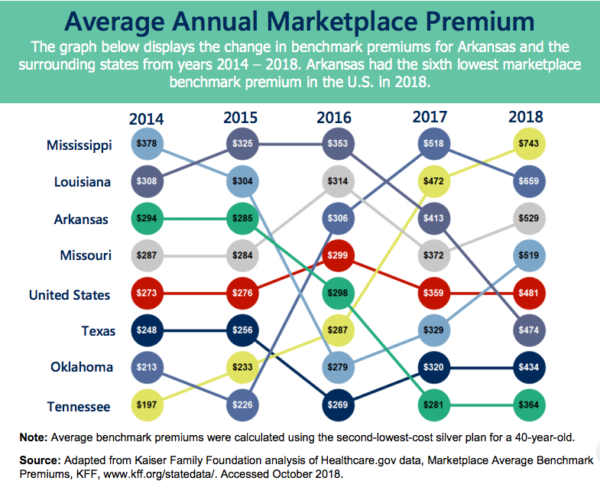
Craig Wilson, the health policy director at ACHI, said in a phone interview that Arkansas’s marketplace rates have remained fairly consistent over the last five years, except for a big jump in 2017. They rose from $281 in 2016 to $364 in 2017 due to the Trump administration’s decision that year to end a type of federal subsidy to insurance companies known as cost-sharing reductions. “Insurers just shifted that cost into the premium price,” Wilson said.
Because Arkansas’s per capita income is lower than most states, it has a fairly high percentage of people who would qualify for generous income-based subsidies. In several counties, the average annual subsidy received by consumers was over $5,000 — high enough to defray most of the cost of a monthly premium. But, Wilson said, many Arkansans still aren’t taking that deal.
“If they take it, they’re likely to get financial assistance,” he said. Many subsidy-eligible people probably aren’t enrolling in low-cost individual coverage because of lack of knowledge, Wilson added. “We haven’t had a lot of consumer outreach on this.” (In 2018, about 68,000 people in Arkansas enrolled in a marketplace plan, according to the Kaiser Family Foundation.)
Arkansas’s marketplace is likely more stable than many other states in part because of Medicaid expansion, Wilson said. When Arkansas expanded Medicaid to cover low-income adults in 2013 — a change made possible under the Affordable Care Act — it was one of the only Southern states to do so. But it approached expansion by creating an unusual hybrid system that provided coverage to people in the expansion population using private plans sold on the marketplace, rather than fee-for-service Medicaid. Under this so-called “private option,” the state used Medicaid dollars to pay the full cost of premiums for low-income people (specifically, those with incomes between 0 and 138 percent of the federal poverty line.)
“I think it’s fair to say that the use of premium assistance in the private market with Medicaid expansion has produced some stability in the individual market, just due to the sheer volume,” Wilson said. There are currently over 250,000 Medicaid expansion beneficiaries in Arkansas who are getting their insurance coverage through a marketplace plan. That “makes it more attractive for insurers to participate in the market and ultimately creates a competitive environment.” He added that having a single large purchaser — Arkansas Medicaid — in the individual marketplace helps put downward price pressure on the rates.
However, Medicaid expansion enrollment has been steadily declining over the past two years. (It’s dropped by almost 80,000 since reaching a peak of 330,000 in January 2017.) In September and October, about 8,500 people lost coverage due to the rollout of a new work requirement for a subset of beneficiaries. In the preceding months, tens of thousands of others were removed from the rolls for other reasons. Some likely moved up the income ladder and found insurance elsewhere; others appear to have lost coverage due to harsher eligibility rules put in place by the state Department of Human Services.
This reporting is made possible in part by a yearlong fellowship sponsored by the Association of Health Care Journalists and supported by The Commonwealth Fund. It is published here courtesy of the Arkansas Nonprofit News Network, an independent, nonpartisan project dedicated to producing journalism that matters to Arkansans. Find out more at arknews.org.