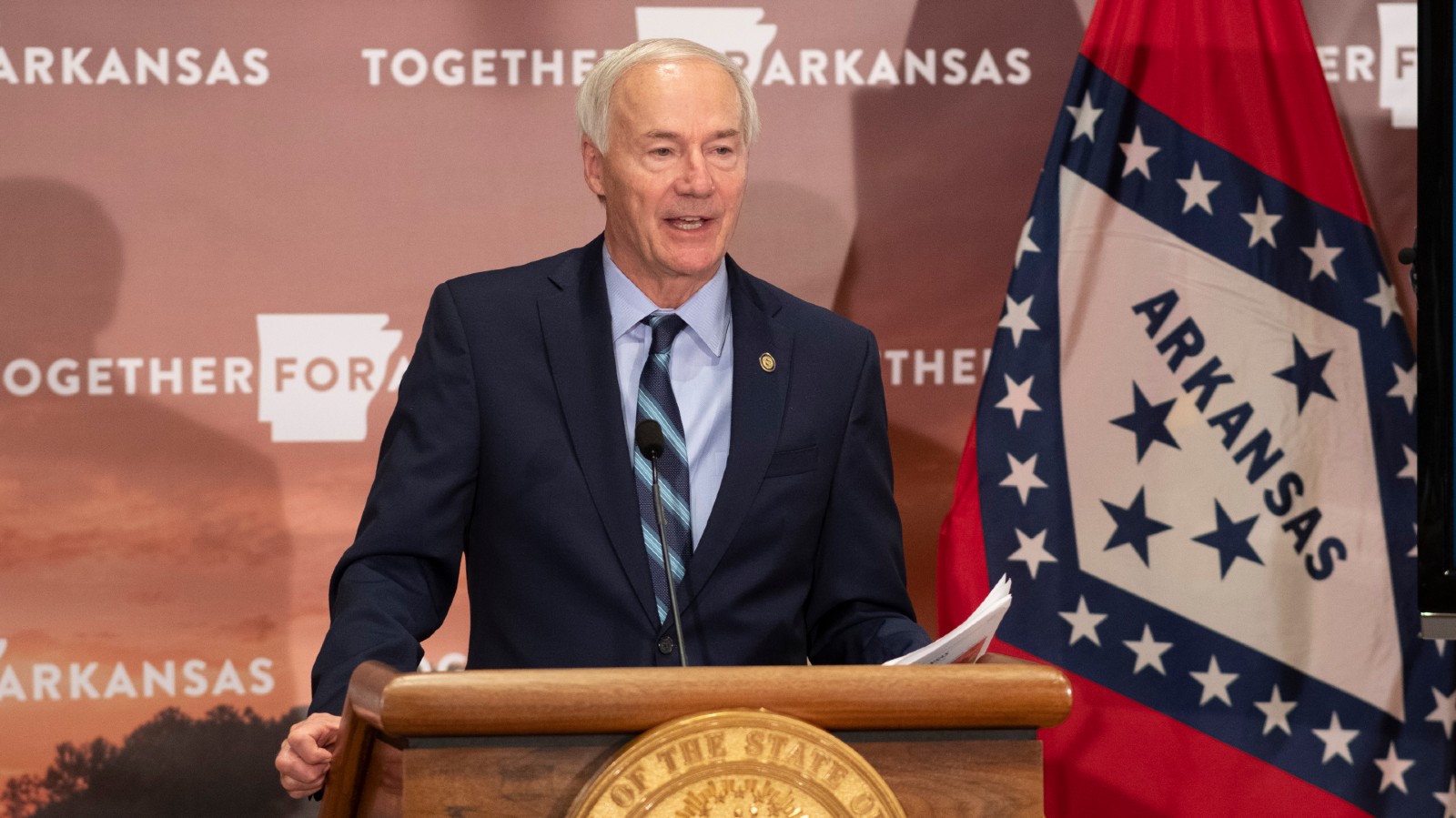
COVID-19 is spreading in Arkansas at rates that a recent University of Arkansas for Medical Sciences report compared to a forest fire, with more than 20,000 active cases as of Monday. The state’s death toll is nearing 3,000.Governor Hutchinson has resisted calls in recent weeks for further restrictions on bars, restaurants, gyms or other non-essential stores and services. At a press conference earlier this month, Hutchinson became animated when reporters repeatedly asked him about the possibility of new restrictions.
“The most important question is: Where are the cases coming from?” Hutchinson said. “The vast majority of cases are coming from social gatherings.” Addressing the media in attendance, he asked, “Would anybody at this table advocate to close down a restaurant if cases are not coming from that restaurant? Or they’re not coming from a particular activity?”
Given the economic pain, Hutchinson argued, tougher restrictions do not make sense because those types of businesses are not a significant source of spread. But the Arkansas Department of Health data that the governor is relying on appears to be too limited and incomplete to reach that conclusion.
Health department investigators call people who test positive for COVID-19 to ask about activities in the two weeks before their diagnosis. But they cannot reach everyone, and no information is available on how many people they have missed — the department does not track the number of cases they failed to reach or the number who were reached but declined to respond to questions. It is often impossible to determine the source of infection for a given case, and the department does not track the total number of infections that occurred in a certain type of business, such as bars or restaurants. If people volunteer information about private social gatherings, interviewers make note of it, but the department does not track specific numbers on such gatherings to confirm the governor’s claim that they produce the “vast majority” of cases.
Health department officials argue that despite these limitations, the data it collects is still revealing.
But Dr. Gary Wheeler, an infectious disease specialist and former chief medical officer of the health department, questioned the conclusion that bars and restaurants have not been a major source of spread.
“The data that’s being collected was not really perfectly designed to collect the information that we’re talking about,” said Wheeler, who retired from the department earlier this month. The governor, he said, needs to ask the department whether its methodology is good enough to determine whether or not the spread of COVID-19 is originating in locations like restaurants and bars. “If it’s not, maybe we should not draw any conclusions from it,” he said.
Wheeler stressed that it has been a couple of months since he was directly involved in the data analysis, but the limitations that concerned him remain in place.
The data is collected by case investigators — typically nurses employed by the health department — who interview Arkansans who test positive for COVID-19. Case investigators ask whether patients have been to certain locations in the two weeks before their diagnosis: restaurants, bars, barbershops, churches, daycares, gyms, health providers, hotels or retail stores (including grocery stores). Investigators also ask whether patients have been in contact with another person infected with COVID-19. Health department officials said investigators make three attempts to reach the patient within a two-day period, but that can vary based on case volume.
The health department publishes reports twice a week that present this data as a percentage. According to the Dec. 14 report, 13% of active cases reported having been to a retail store, 3% reported having been to a restaurant and just 0.1% (22 people total) reported having been to a bar. All other listed activities are at or below 3%.
But 3% of what? The health department is calculating the percentage based on all active COVID cases (the denominator in the department’s equation), not those people who actually responded. That means it’s including people who never answered the question or never even picked up the phone. And it’s including new cases from patients who have not yet been called by investigators. Because the department does not track those numbers, there is no available information on the relevant question: Among those who actually responded, what percentage engaged in various activities?
Asked about these gaps in the data, health department spokesman Gavin Lesnick said, “We believe the information in the report is still relevant, while taking into account [these] limitations.”
“The denominator should be the people who have participated in the case investigation,” said Dr. Amesh Adalja, an expert in infectious disease at the Johns Hopkins Center for Health Security. “You want to make sure the denominator matches the actual responses.”
To determine the value of the data, Adalja said, it’s important to acknowledge the number of people the data never captured, which could lead to missing potential sources of infection.
Mike Cima, the health department’s chief epidemiologist, was not able to provide a specific estimate but said that the department reaches the majority of people, and that most of those who are reached respond to the questions about recent activities.
“I do not believe that it is a pervasive issue that we are not collecting this information on large swaths of people — I don’t think that’s happening,” Cima said. “I think we are actually getting in contact with the majority of our cases and we’re getting the information that we need.”
Another problem is that to draw conclusions with confidence, researchers want to make sure the sample of people they are speaking with isn’t somehow unusual or distinct from the overall pool of active cases.
“People who don’t respond are probably very different than the people who do respond to the health department,” Adalja said. “It’s probably not random. So you get a skewed picture.”
Cima acknowledged that it was “likely that at least some degree of [what is missing from the sample] is not truly random.”
In addition to the unknown number of people who never responded, never answered or haven’t been called, around 5% of current active cases are people in jails, prisons or nursing homes. They are likewise included in the denominator, but would not typically be asked the questions about activities in the weeks prior to diagnosis.
Because of the various factors driving the percentages down, the health department data paints a strange picture. The chart it publishes, which has previously been cited by the governor, shows only tiny fractions participating in various activities, and just 13% who have even been to any retail store, including the grocery store. As presented, it seems to imply that people who contracted COVID-19 rarely left their homes in the two weeks before they tested positive. That would be a curious finding, unless people who wind up getting COVID-19 are much more cautious than others. Mobility data released by Google suggests that trips to such locations are down only slightly from the pre-COVID baseline.
“It’s possible that [the percentages] are somewhat conservative,” Cima said. Still, he said, the data gives the department some useful information about the spread of the virus.
Even if someone provides detailed and accurate information about their activities, case investigators often may not have enough information to determine the source of infection.
“Asymptomatic and pre-symptomatic spread makes it difficult to know with certainty in every case,” Lesnick said. “Some individuals visit multiple locations prior to infection, and establishing the precise point of transmission is impossible.” As the virus becomes increasingly widespread, people may have multiple exposures to infected people without even knowing it.
Sometimes, there’s not even a clue to work with. Since the beginning of the pandemic, in more than a third of all cases (inclusive of those who were never reached), investigators were unable to identify any link at all to another case.
The health department acknowledges other confounding factors that could further complicate efforts to identify the source of infection. People are more likely to be aware of links to people they interacted with in the home or at social gatherings than people they encountered at a restaurant or in a store. Data analysts could be misled by low-hanging fruit: Respondents would know if an uncle at Thanksgiving tested positive, but might never learn about the stranger they sat next to at a bar.
People may also be reluctant to reveal certain activities to investigators, particularly if they are perceived to be contrary to COVID safety precautions. “It would be safe to say some degree of social norm bias would be happening,” Cima said.
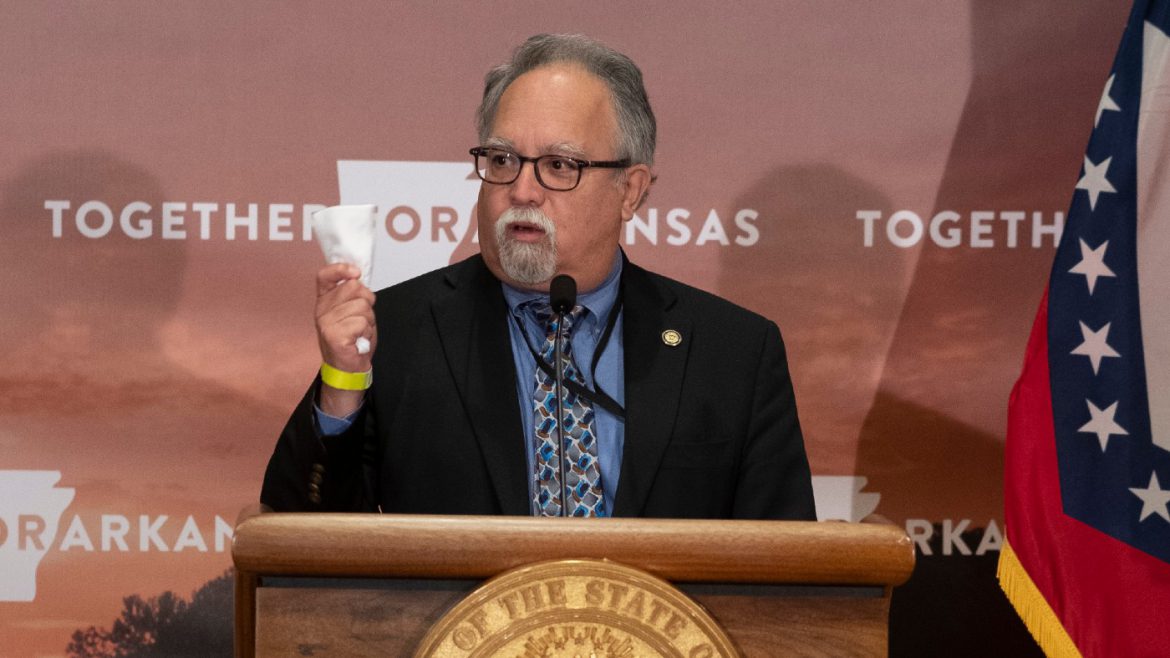
“We rely, quite honestly, on the honesty and forthrightness of people,” state Secretary of Health Dr. Jose Romero said. “If they don’t want to tell us [where they’ve been], we can’t extract the data.”
Asked whether the data — despite its various limitations — was sufficient to conclude that locations such as bars, restaurants and gyms were not a significant source of spread, Cima said, “I would not use the word ‘conclusive’ in any direction whatsoever.” Some transmission could be occurring there, he said. “I think it would be naive to say no,” he said. “Are those accounting for the large swath of cases that are occurring right now? I do not believe so.”
Wheeler, the former health department official, was skeptical that the existing data is enough to indicate that bars and restaurants are not a significant source of spread in Arkansas.
“Why are we different from everywhere else?” Wheeler asked. “Because in other studies that have been done, it’s been clear that restaurants, bars, etc., are very fertile places for the spread of disease. I’ve been to bars and restaurants in other states and other places and they’re kind of the same.”
Wheeler pointed to a recent study in the science journal Nature that used cell phone data to map people’s movements in 10 U.S. cities and found that venues such as restaurants and gyms appeared to be major hotspots for transmission. Regional variation could be possible, Wheeler said, but given the clear scientific reasoning behind the possibility of transmission in such locations, more robust data would be necessary to support the conclusion that Arkansas was an outlier.

Cima pointed instead to social gatherings as the dominant culprit. Despite the governor’s claim that the “vast majority” of cases come from social gatherings, the health department does not collect hard numbers on such activities. Patients are not asked specifically about whether they have attended birthday parties or barbecues. Instead, Cima said, the department analyzes qualitative data, in the form of information that people may share when they are asked about any close contact with someone who has tested positive.
Case investigators have an open field in the form in which they can record details that respondents volunteer regarding social activities. Department analysts then might hunt for certain keywords, like “Thanksgiving” or “party,” to identify trends in the behavior of recently infected people, Cima said.
Cumulatively, Cima said, this anecdotal data suggests a pattern of spread at social gatherings, particularly when paired with spikes in cases seen around major holidays. “I think that the social gatherings, the indoor holidays, the indoor celebrations and not social distancing and wearing masks is the largest contributing factor to the spread of COVID-19 in Arkansas,” he said.
Wheeler said that the health department and nurse investigators were doing the best they could with limited resources. “But the conclusions that you draw from your data are based on the quality of data that goes in,” he said. “And if you’re not getting great data, then your conclusions may not be that strong.”
At times, Hutchinson himself has explicitly noted the holes in the data. “As governor I always wish I had better data,” he said Dec. 1. “I wish I knew exactly the source of every positive case so I could say, ‘Here it is, there’s a problem, we can address it there.’ But the data is not that good, much of it is human data. … It’s not always clear as to where that case came from.”
For the governor, the lack of more detailed information on the source of infection is reason not to impose additional restrictions. After all, if the data doesn’t rule out the possibility that places like bars and restaurants are a major source of spread, it doesn’t prove that they are, either.
“That’s why I’ve always said let’s don’t put economic restrictions on people and restrict their ability to make a living unless we have good data and understand the consequences of it,” he said. Last month, the governor imposed an 11 p.m. closing time on venues that serve alcohol, but otherwise has kept the same regulations that have been in place since June, limiting occupancy to 66 percent and establishing safety protocols but allowing indoor dining and bars to remain open.
Wheeler said the governor should consider further restrictions, even if the state is operating with limited data, because such interventions have proved effective at slowing the spread of the virus.
“The major argument that underlies this whole discussion is: Are we doing well or are we not?” Wheeler said. “Well, we’re not doing well, and we’ve done essentially no interventions other than this 11 o’clock curfew that the governor put in. And the numbers continue to climb. So should we not try what has been used in other places? In general, if you look at other countries or states that have successfully brought their numbers down, it includes almost universally cutting back on the in-house dining, closing of bars and that kind of thing.”
One of the places that had success with aggressive restrictions, Wheeler said, was Arkansas last spring, when the state ordered many non-essential businesses to close on March 20.
“Just to remind the governor, he did this once,” Wheeler said. “And it worked.”
Asked directly at a press conference Tuesday whether the health department data was sufficient to support his conclusions about the source of infection, Hutchinson deferred to Cima.
Cima summarized the health department’s case investigation questions, and noted “social gathering information [that] is qualitative in nature.”
After the press conference, a reporter asked Romero, the health secretary, if he would eat at a restaurant.
“I haven’t eaten in a restaurant in months,” Romero said. “Would I go to a department store to browse? No. Would I go anywhere I don’t have to go? No.” Cima also replied no.
Leslie Peacock contributed reporting for this story.
This reporting is courtesy of the Arkansas Nonprofit News Network, an independent, nonpartisan news project dedicated to producing journalism that matters to Arkansans.