In June 2018, when Arkansas became the first state in the nation to implement work requirements for certain Medicaid beneficiaries, Governor Hutchinson was triumphant.
“We’ve wanted to establish a work requirement … for a long time,” he said at the time. The Obama administration had refused to authorize work requirements, but the Trump administration gave the green light. “With this development, Arkansas has become a national leader in rethinking the delivery of public assistance,” the governor boasted.
Three and a half years later, the work requirements are gone. The state did not even ask to continue the policy after the Biden administration signaled early in 2021 that it would no longer allow Medicaid work requirements. The Biden administration officially revoked the state’s authorization in March; by that point, the policy had already been blocked for two years by a federal judge.
Last week, the Biden administration established another red line. On Dec. 21, the federal government approved a proposal from Arkansas officials to continue the state’s unique version of the Medicaid expansion program, but the feds rejected Arkansas’s request to continue imposing monthly premiums on certain beneficiaries. The premiums will be allowed to continue for one more year before ending on December 31, 2022.
The Medicaid expansion, authorized by the federal Affordable Care Act, covers adults aged 19-64 who make less than 138% of the federal poverty level (an annual income of $17,774 for an individual or $36,570 for a family of four). Ideological opposition to Obamacare has led to fierce debates in red states over whether to expand Medicaid, and a dozen states still have not done so. Some Republican governors, like Hutchinson, have been willing to take the federal money for coverage expansion — but have sought to bend the program in various ways, including imposing requirements on beneficiaries that critics allege create barriers to coverage and reduce the number of people enrolled.
Federal law allows states to experiment with new policies that deviate from Medicaid rules under agreements known as waivers, but such programs require federal approval. In an executive order last January, the Biden administration announced it would review Medicaid waiver policies “that may reduce coverage under or otherwise undermine Medicaid or the ACA.”
Work requirements were the first shoe to drop. Now, the Biden administration has made clear it will not allow premiums to be imposed on beneficiaries in the Medicaid expansion population, nixing proposals to continue premiums from both Arkansas and Montana on Dec. 21. In both cases, the Biden administration gave a one-year off ramp before premiums will end.
Three other states currently have waivers for Medicaid expansion premiums, according to tracking by the Kaiser Family Foundation. (Another such waiver is pending, and another has been currently set aside by a court ruling.) Presumably, the Biden administration will not renew such provisions or allow new requests for premiums from other states.
The novel version of the Medicaid expansion program in Arkansas, first enacted in 2014, uses Medicaid funds to purchase private health insurance plans on the Arkansas Health Insurance Marketplace — the regulated marketplace created by the ACA — to cover most beneficiaries. Once nicknamed the “private option” and now known as “Arkansas Works,” it has been implemented under a series of waiver agreements with the federal government.
The “Arkansas Works” waiver expires at the end of this year. Arkansas’s request for a new waiver, submitted last summer, renamed the program ARHOME and outlined new changes and policy initiatives.
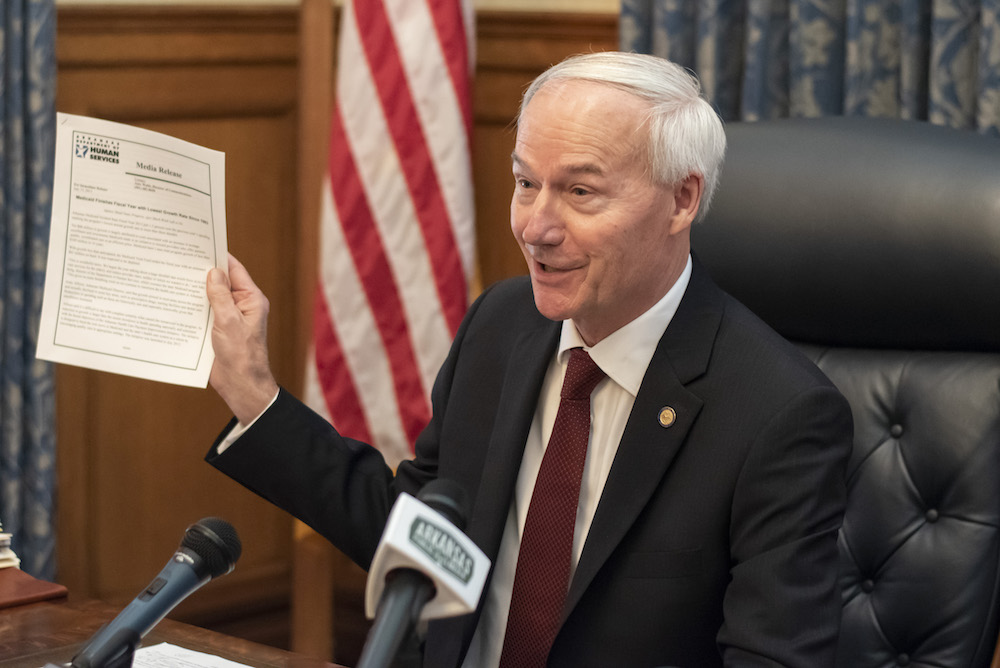
Despite the rejection of the state’s request on premiums, Governor Hutchinson described the feds’ overall approval of ARHOME as “good news” in a press conference on Dec. 21. “This will allow 300,000 low-income Arkansans to continue to receive health care,” Hutchinson said.
The governor said the Biden administration’s decision against allowing premiums in ARHOME was “not unexpected,” despite the state’s efforts to convince federal regulators otherwise. “We continue to believe it is important for nonelderly, nondisabled adults to contribute to the cost of their coverage,” Hutchinson said in an email this week.
The governor noted that beneficiaries still may incur some costs even after premiums are phased out. Small co-pays are allowed under Medicaid rules, with certain limitations. (Premiums are monthly payments made at a set rate, whereas co-pays are assessed when a medical service is actually used.)
Arkansas Works currently charges co-pays to most beneficiaries who make more than the federal poverty line. The state’s ARHOME waiver request proposed allowing co-pays to be charged to some beneficiaries with lower incomes (down to 21% of the federal poverty level) and raising the caps on the total quarterly amounts that can be charged to those at higher incomes, among other changes. State officials hope to implement the updated co-pays — which will follow normal Medicaid rules — this year, pending approval from the state legislature and the Biden administration.
Arkansas had received permission for premiums under its previous waiver agreement, which was approved by the Obama administration. (After Trump took office, the waiver was amended to include work requirements, approved in 2018.) But the Centers for Medicare and Medicaid Services (CMS), the federal agency overseeing Medicaid, “has since determined that premiums can present a barrier to coverage,” according to a letter CMS Administrator Chiquita Brooks-LaSure sent to the state last week.
Premiums for Medicaid expansion beneficiaries “are not likely to promote the objectives of Medicaid,” Brooks-LaSure wrote in the letter, which accompanied the federal approval for ARHOME.
Joan Alker, the executive director of Georgetown University’s Center for Children and Families, said that CMS made the right decision.
“For low-income populations, it’s very clear that premiums reduce participation,” Alker said. “There’s lots of research to back this up: When premiums are imposed, enrollment goes down. In our system having insurance is the price of admission, so we’re just kicking people out of the system.”
Currently, the state imposes $13 per month premiums on most beneficiaries who make more than the federal poverty line ($12,880 for an individual or $26,500 for a family of four). Beneficiaries do not lose coverage for failure to pay, but incur a debt to the state, which can be withheld from state tax refunds.
Alker said premiums can still be a barrier to coverage even if the state doesn’t kick people off Medicaid for failing to pay. People might be reluctant to sign up in the first place or worry about accruing debt for bills they can’t afford.
“Any premium is acting as a deterrent to enrollment,” she said. “If people think they have to pay a premium and they don’t have the money, they probably haven’t read the fine print.”
The waiver proposal for ARHOME that the state submitted earlier this year described a plan to increase premiums in 2022 to between $22 and $27 for those above the poverty line, depending on income. Failure to pay would still not have led to a loss in coverage, but would have incurred a debt to the insurance companies rather than the state.
CMS will allow the state to continue charging premiums to beneficiaries above the poverty line for one more year to allow “a planned phase-out of the policy,” giving Arkansas time to communicate the change to beneficiaries and make necessary operational changes. State officials said the current $13 per month premiums will continue through 2022. (From this point forward, any debt for unpaid premiums will be up to the insurance companies to collect, rather than the state. However, both the old waiver and the new waiver prohibit reporting the debt to credit bureaus, referring the debt to collection agencies, or taking legal action to collect the debt.)
Medicaid waivers like ARHOME are intended to allow states to experiment with new initiatives to further the objectives of the Medicaid program. States are supposed to evaluate these demonstrations or pilot programs to test a hypothesis about the benefits of policies like premiums or work requirements. In her letter to the state, Brooks-LaSure wrote that the decision to deny authorization for premiums was informed by research in other states with similar waiver programs, which showed that the premiums “resulted in shorter enrollment spells, and were associated with lower initial enrollment rates and increased obstacles to accessing care in several states.”
In Arkansas, Brooks-LaSure wrote, the state’s evaluation of Arkansas Works likewise indicated that “beneficiaries had shorter, but more frequent gaps in coverage.”
Brooks-LaSure added that “premium requirements can exacerbate health disparities,” pointing to research from several states that showed the barriers to enrollment created by premiums were worse for Black beneficiaries and lower-income beneficiaries.
The ARHOME agreement with the feds will go into effect on January 1 and run through 2026. It will continue to use private insurance plans to cover most beneficiaries. In addition to the changes to co-pays, the state’s proposal outlines a number of other new features, including: incentives to encourage wellness and “economic independence” in the form of small rewards offered by the private plans; moving beneficiaries to traditional Medicaid if they are deemed “inactive,” meaning they don’t use their private health plan at all; a reduction in retroactive Medicaid coverage for new enrollees from 90 days to 30 days; efforts to hold the insurance companies accountable in terms of health outcomes, as well as mechanisms to curb cost growth for the insurance plans; and new programs for rural health, maternal and infant health, behavioral health and certain at-risk populations. Some of these new initiatives are still in development and will require additional federal approval.
Two days after the feds rejected premiums in Arkansas and Montana, the Biden administration rescinded the authority for work requirements (as well as premiums) for a Medicaid waiver in Georgia that had been approved by the Trump administration. Georgia was the last state that still had waiver authority for Medicaid work requirements, though the state had not yet implemented the policy. The Biden administration has now formally revoked approval in ten states, according to the Kaiser Family Foundation, with other states withdrawing after receiving approval.
The Arkansas work requirements have been suspended since a federal judge halted the policy in March 2019. The program required certain beneficiaries to report their hours worked each month to the state Department of Human Services; if they were not working, they could instead report participation in job training programs, job searches or certain approved volunteer activities. If beneficiaries failed to comply, they would be kicked out of the program and lose coverage. Over the course of 5 months in 2018 and 2019, more than 18,000 Arkansans lost their health insurance due to the policy before it was halted by the federal courts.
State officials aren’t giving up on work requirements in the future, even if the policy is dormant for now: In the waiver proposal for ARHOME, Arkansas officials stated their intent to seek an amendment to the waiver “if federal law or regulations permit the use of a work and community engagement requirement as a condition of eligibility in the future.”
The only trace of the policy that remains in the current incarnation of ARHOME: Beneficiaries may earn small rewards from the private insurance companies for participating in health improvement or work-related activities. The insurance companies are required to offer four wellness-related incentives and one for “economic independence.”
“The rewards may be redeemed in the form of a gift card, which beneficiaries will have several options to choose from,” said Max Greenwood, vice president of government and media affairs for Arkansas Blue Cross Blue Shield, one of the insurance companies that provides coverage to Medicaid expansion beneficiaries. “Beneficiaries can earn rewards ranging from $15 to $200, and also may be eligible for multiple rewards in any given benefit year.”
This story is courtesy of the Arkansas Nonprofit News Network, an independent, nonpartisan news project dedicated to producing journalism that matters to Arkansans.